Real-Time Feedback Devices In ACLS: Boosting Life-Saving Skills
Saving a life often comes down to quick, accurate actions, and when it comes to advanced cardiac life support, or ACLS, every single second truly counts. We're talking about situations where someone's heart has stopped, and immediate, effective help is needed right away. That's why the tools we use for training and actual care are so important, and there's a growing buzz about how real-time feedback devices in ACLS are making a huge difference, you know.
For a long time, learning CPR and other emergency procedures relied a lot on instructors watching and telling you what to do. But now, with newer technology, we have devices that can actually tell you, right then and there, how well you're doing. This means you get instant information on things like chest compression depth and rate, which is, honestly, a pretty big deal for learning and for patient care.
This article is going to explore what these real-time feedback devices are all about, how they work, and why they're becoming such an important part of ACLS training and practice. We'll also look at what to consider if you're thinking about using them, and, basically, what the future might hold for these helpful tools.
Table of Contents
- What Are Real-Time Feedback Devices in ACLS?
- How These Devices Work to Help
- Why Real-Time Feedback Matters for ACLS
- Key Features to Look for in a Device
- Improving Training and Patient Care with These Tools
- Choosing the Right Device for Your Needs
- Common Questions About ACLS Feedback Devices
- Looking Ahead: The Future of ACLS Support
What Are Real-Time Feedback Devices in ACLS?
Real-time feedback devices in ACLS are, put simply, gadgets that give you immediate information about the quality of the life-saving actions you're performing. Think of them as a personal coach, but one that provides data instantly, as you're doing something. This is pretty useful, actually, for anyone involved in emergency medical care.
These tools usually come with sensors that can measure different aspects of resuscitation efforts. For example, during CPR, they can tell you if you're pushing deep enough on the chest, if you're pushing fast enough, and if you're allowing the chest to fully come back up between compressions. This immediate insight is, you know, a game-changer for learning and doing.
The idea behind them isn't totally new, but the technology has gotten much better recently. Early versions might have just given a simple "good" or "bad" signal, but today's devices offer a lot more detail, which is certainly a step up.
They aim to make sure that the care given during a cardiac arrest is as effective as possible. Because, quite frankly, poor quality CPR often doesn't help as much as it should, and that's a problem we're all trying to fix.
These devices are, in some respects, a way to standardize care. Everyone gets the same objective information, which helps bring everyone's skills up to a similar, high level. It's a really practical approach to improving patient outcomes, so.
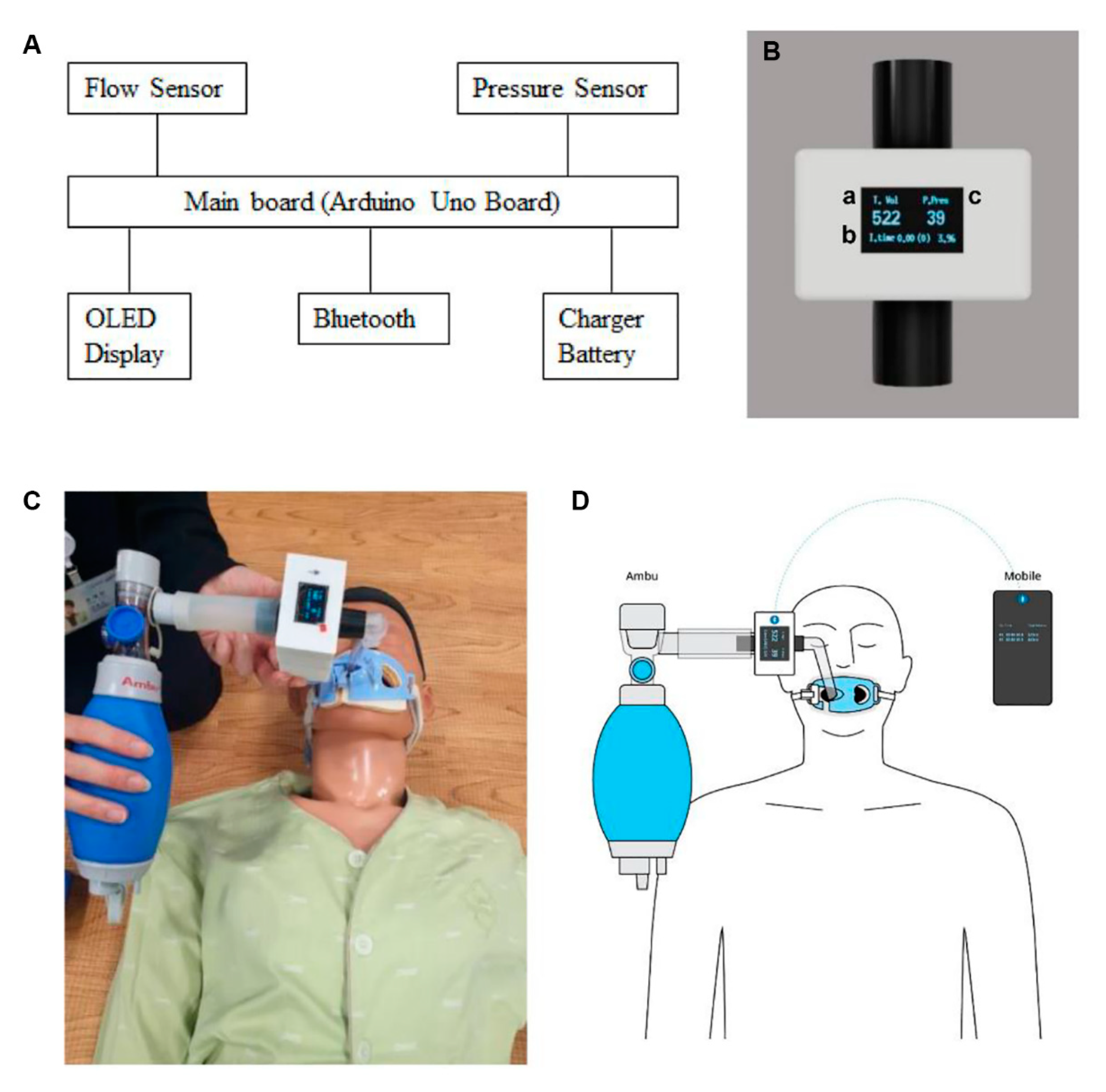
Components and How They Help
Most of these devices have a few main parts. There's usually a sensor that attaches to the patient or a training mannequin, and then a display unit that shows the information. The sensor is the part that collects all the data, like how much pressure is being applied or how quickly it's happening, you know.
The display can be something as simple as a series of lights, or it could be a small screen showing numbers and graphs. This visual feedback is really important because it lets the rescuer see what's happening without having to stop what they're doing. Some devices even offer auditory cues, like beeps, to guide the rate of compressions, which is pretty clever.
These different types of feedback help in various ways. Visual cues give detailed metrics, while auditory cues can help maintain a steady rhythm. It's almost like having a metronome for your chest compressions, which, honestly, can be very helpful when you're under pressure.
Some devices also track ventilation rates and volumes, making sure breaths are delivered correctly. This comprehensive approach means that rescuers get a full picture of their performance, which is, in fact, incredibly valuable for overall resuscitation efforts.
The goal is always to provide actionable information that helps the rescuer adjust their technique right away. This immediate correction is what makes these devices so effective for improving skills, so it's a bit different from getting feedback much later.
How These Devices Work to Help
The core function of these devices revolves around monitoring and guiding the quality of CPR. When someone is doing chest compressions, the device's sensors measure things like the depth of each push and the rate at which they are happening. It also checks for full chest recoil, meaning the chest comes completely back up after each compression, which is actually super important for blood flow.
This information is then processed instantly and shown to the rescuer. If compressions are too shallow, the device might show a red light or a message saying "push deeper." If they're too fast or too slow, it could give a different signal. This immediate guidance helps the rescuer adjust their technique on the spot, which is really beneficial, you know.
Beyond CPR, some advanced devices can also help monitor other vital signs during a simulated emergency. They might track heart rhythms or blood pressure in a training scenario, providing a more complete picture for the learner. This broader scope helps in understanding the full context of an ACLS situation, which is, frankly, pretty neat.
The idea is to give objective, data-driven feedback that takes the guesswork out of resuscitation. Human observation can be subjective, but a machine measuring physical actions provides consistent, unbiased information, which is, in some respects, a big advantage.
This consistent feedback helps build muscle memory and good habits. Over time, rescuers who train with these devices tend to develop better, more consistent CPR skills, which is, obviously, the whole point.
The Technology Behind the Scenes
At the heart of these devices are clever sensors, usually accelerometers or force transducers. These tiny components are very good at detecting movement and pressure. When you push on a chest, they translate that physical action into electronic signals, you know.
These signals then go to a small computer inside the device. This computer runs special software that compares the incoming data to established guidelines for good CPR, like those set by medical organizations. This comparison happens in milliseconds, which is, honestly, pretty fast.
The immediate display for users is a key part of the technology. Whether it's a simple LED display or a more detailed screen, the information has to be easy to read and understand at a glance, especially during a stressful situation. This user-friendly interface is, in fact, a crucial design element.
Some devices can also record the data from a resuscitation attempt. This means that after the event, whether it's a training session or a real emergency, instructors or medical teams can review the performance. This post-event analysis is, basically, another layer of learning and improvement.
The ongoing development in this area means devices are getting smaller, more accurate, and more integrated with other medical equipment. It's almost like they're becoming smarter and more helpful with each new version, which is, you know, a good thing for everyone.
Why Real-Time Feedback Matters for ACLS
The main reason real-time feedback matters so much for ACLS is simple: it leads to better patient outcomes. When CPR is performed well, the chances of someone surviving a cardiac arrest go up significantly. These devices help ensure that "well" happens more often, so.
Without immediate feedback, a rescuer might be performing CPR that feels right but isn't actually effective. They could be pushing too softly, or not letting the chest fully rise. The device catches these issues right away, allowing for immediate correction, which is, frankly, incredibly important.
It also brings a level of consistency to training that was harder to achieve before. Every student gets the same objective assessment of their skills, rather than relying solely on an instructor's observations, which can vary a bit. This standardization is, in some respects, a huge benefit for widespread training programs.
The stakes in ACLS are incredibly high. We're talking about life and death. So, any tool that can improve the quality of care delivered during these critical moments is, honestly, a valuable addition to our medical toolkit.
This kind of feedback helps build confidence in rescuers, too. Knowing that you're performing CPR correctly, or getting the guidance to correct it, can make a big difference in a high-stress situation. It's like having a little extra reassurance when you need it most, you know.
Benefits for Learners and Educators
For people learning ACLS, these devices make skill acquisition much faster and more effective. Instead of waiting for an instructor to comment, you get instant cues. This means you can practice, adjust, and improve your technique much more quickly, which is, basically, how people learn best.
The objective assessment provided by the devices takes away some of the guesswork. Learners can see their progress in clear numbers and graphs, making it easier to understand where they need to improve. This data-driven approach is, in fact, very motivating for many students.
Educators also get a lot out of these tools. They can see exactly how each student is performing, allowing them to focus their teaching on specific areas where a student might be struggling. It frees them up to coach more effectively, rather than just observing, which is pretty useful.
These devices help standardize teaching methods across different instructors and different training sites. Everyone is working towards the same measurable goals for CPR quality, which means a more consistent level of training for everyone involved. This consistency is, frankly, a big win for medical education.
They also provide valuable data for debriefing sessions after training scenarios. Instructors can show students exactly what happened during a simulated cardiac arrest, highlighting moments of excellent performance and areas that need work. This detailed review is, honestly, a powerful teaching tool, so.
Key Features to Look for in a Device
When you're considering real-time feedback devices for ACLS, there are a few things you'll want to keep in mind. First off, accuracy is paramount. The device needs to give precise measurements of compression depth, rate, and recoil, because, you know, inaccurate feedback isn't helpful at all.
Ease of use is another big one. In an emergency, or even during a training session, you don't want a device that's complicated to set up or understand. It should be intuitive, with clear visual or auditory cues that are easy to interpret quickly, which is, in fact, pretty important.
Durability is also a consideration, especially if the device will be used frequently or in various settings. It needs to withstand the rigors of training and potentially real-world use. A good battery life is also very helpful, so you're not constantly worrying about recharging, which is, honestly, a bit of a hassle.
You'll also want to think about whether the device is designed for adult, pediatric, or infant CPR, or if it can do all three. Some devices are versatile, while others are more specialized. Matching the device to your specific training or clinical needs is, basically, a smart move.
Finally, consider the overall cost and any ongoing support or maintenance needs. Like any piece of equipment, there might be software updates or calibration requirements. Understanding these aspects beforehand can save you headaches later, you know.
Important Considerations
When picking out a real-time feedback device, compatibility with your existing training equipment or defibrillators can be a factor. Some devices integrate directly with mannequins or AEDs, offering a more streamlined experience, which is, frankly, pretty convenient.
Data logging capabilities are also worth thinking about. If you want to track individual performance over time or review group results, a device that records and stores data is going to be really useful. This allows for long-term skill development and quality improvement, which is, in some respects, a big benefit.
Consider the type of feedback it provides. Is it just visual, or does it also offer auditory cues? Some people learn better with one type of feedback over another, so having options can be good. A device that offers both might be, honestly, a very versatile choice.
The cost, of course, plays a role. These devices range in price, and what might be suitable for a small training center could be different from what a large hospital system needs. It's about finding the right balance between features and budget, you know.
Lastly, look into the manufacturer's reputation and customer support. Knowing that you can get help if you have questions or issues with the device is, basically, peace of mind. A reliable company often means a reliable product, so.
Improving Training and Patient Care with These Tools
These devices are truly making a difference in both how we train for ACLS and how we provide actual patient care. In simulation settings, they give learners an objective way to practice and refine their skills, which is, frankly, invaluable. It's like having a constant expert observer telling you exactly what to do better, right then.
When it comes to real-life emergencies, some defibrillators and monitors now come with integrated real-time feedback. This means that during an actual cardiac arrest, the medical team gets immediate data on their CPR quality. This can help them adjust their technique on the fly, potentially improving the patient's chances of survival, which is, honestly, pretty amazing.
The gap between practice and real life is often a big challenge in medicine. These tools help bridge that gap by providing consistent, data-driven performance metrics in both environments. What you learn in training directly translates to what you do in an emergency, which is, in some respects, a huge step forward.
They help reduce the variability in CPR performance that can happen when different people are providing care. With a feedback device, everyone gets the same objective standard to aim for, leading to more consistent, high-quality chest compressions. This

Audiovisual Feedback Devices for Chest Compression Quality during CPR

Introducing the Audible CPR Feedback Device That Fits in the Palm of
Medicina | Free Full-Text | Effectiveness of a Real-Time Ventilation